
As I begin my year as president of ACCP, I would like to take some time to reflect on several important aspects of the “who,” “what,” “how,” and “why” of our practice. My perspective comes from that of a clinician whose primary role is at the bedside in a medical-surgical critical care unit. As clinicians with high standards, we provide comprehensive medication management (CMM), possess advanced education and training―including accredited residency training and board certification, and practice as part of a collaborative health care team. In an increasing number of settings, we are credentialed and privileged for specific direct patient care responsibilities. Although the definition of a clinical pharmacist is fairly specific, it does not adequately capture our ability to make a difference for our patients and professional colleagues, the “who” of our practice. Our attitude and expectations set us apart from many other pharmacists. We assume responsibility for the pharmaceutical care of our patients, ensuring that we do more than just make recommendations for the optimal drug therapy―we also follow through to complete the implementation of our recommendations.
The growing roles of board-certified practitioners further emphasize our commitment to self-development and competence assurance. Today, there are almost 20,000 board-certified practitioners (http://bpsweb.org/news/factsheet.cfm), most of whom are pharmacotherapy specialists. Achievement of board certification is an important step toward differentiating practitioners and enabling credentialing for specific responsibilities. Personally, I’m excited for the opportunity to become certified in critical care pharmacy practice next year, and my colleagues who practice in pediatric settings are similarly preparing for their exams. The 2015 ACCP Certification Affairs Committee will be evaluating and helping the Board of Regents prioritize other potential areas to recommend to the Board of Pharmacy Specialties for specialty or subspecialty recognition in the future.
California is currently writing regulations to support legislation defining advanced practice pharmacist (APP) (http://leginfo.legislature.ca.gov/faces/billNavClient.xhtml?bill_id=201320140SB493 Key provisions for APP recognition include two of the following three criteria: (1) certification in a relevant area of pharmacy practice, (2) completion of a postgraduate residency, and (3) completion of at least 1 year of practice in a collaborative practice environment. Practitioners recognized as APPs may perform patient assessments, order and interpret drug therapy–related laboratory tests, refer patients to other providers, participate in the management of diseases in collaboration with other health care providers, and initiate, adjust, or discontinue drug therapy. Having established specific criteria for advanced practice, U.S. Public Health Service and Veterans Affairs pharmacists already possess local privileges for prescribing, and the models used are expected to be a resource as individual states address similar approaches to clinical pharmacy practice. Work continues on the national level for the recognition of qualified clinical pharmacists who provide CMM.
It has been important to ACCP to define exactly “what” clinical pharmacists do, and this is well described for both pharmacy and non-pharmacy audiences in the College’s Standards of Practice for Clinical Pharmacists, released on the ACCP Web site in April 2014 and recently published in Pharmacotherapy (see http://www.accp.com/docs/positions/guidelines/StndrsPracClinPharm_Pharmaco8-14.pdf). A general Pharmacist Process of Care was also recently published by the Joint Commission of Pharmacist Practitioners (JCPP)―a collaborative that includes 11 national pharmacy organizations, including ACCP (see http://www.ACCP.com/docs/positions/misc/JCPP_Pharmacists_Patient_Care_Process.pdf). This document defines the steps of a patient-centered approach to collaborative care for all pharmacists (see a graphic depiction in the figure that follows). The components of collection, assessment, planning, implementing, and monitoring/evaluating the needs of patients are not new to clinical pharmacists. Similarly, the components of communication, collaboration, and documentation are core to the clinical pharmacist’s care process but may currently be missing in many of today’s pharmacy practice settings. Still, JCPP’s articulation of this process of care serves as a landmark step toward leading the profession to an envisioned future where pharmacists routinely contribute to optimal medication therapy outcomes.
Because individual state scopes of pharmacy practice may well hinder pharmacists from fully implementing the JCPP process of care in some settings, state pharmacy associations and ACCP chapters should work to ensure that local regulations don’t impede its implementation. In addition, I challenge today’s practitioners to evaluate their own practices to determine whether they fully adhere to this process of care and to implore their administrators and colleagues to make this type of practice an expectation of all pharmacists. Moreover, faculty in our schools and colleges of pharmacy should ensure that students are adequately prepared to employ this process of care and then master it during postgraduate training. We need to be consistent in our approach to team-based, patient-centered care, despite the challenges found in many practice environments. In this regard, the profession will have to continue being creative in its use of technology and qualified support personnel.
My theme of the year, “Advancing Our High Standards of Practice for Clinical Pharmacy,” is based on ACCP’s Standards of Practice for Clinical Pharmacy. In addition to clearly defining the clinical pharmacist’s process of care, the Standards document elaborates on the qualifications, documentation, and collaborative/team-based practice required to provide CMM. Although some clinicians may lament that it took so long to publish this document, the Standards provides a principle to which clinical pharmacists can fully subscribe. And hopefully, this document will finally allow my mother (and others!) to better understand what I do every day. This is the yardstick by which to measure our practice and, as such, poses some significant challenges. As a critical care clinician caring for very complex patients with numerous preexisting conditions that are exacerbated by acute clinical decompensation, I have found that documenting how I provided CMM can be a time-consuming component. I challenge practitioners to be creative in the design of their documentation processes. From the inefficiencies in the current electronic health record, we need to learn how to be more effective in documenting our activities. In accordance with this effort, the 2015 ACCP Clinical Practice Affairs Committee will provide recommendations for implementing these standards and providing meaningful documentation.
“How” we practice as members of a collaborative acute care team has been recognized by the American College of Physicians, and we continue to work with several physician organizations to foster recognition of our role on the acute care team (see Doherty RB, Crowley RA. Principles supporting dynamic clinical care teams: an American College of Physicians position paper. Ann Intern Med 2013;159:620-6).
In addition, I need to emphasize the importance of the “why” in clinical pharmacy practice and the important role of ACCP. In his book Start with Why: How Great Leaders Inspire Everyone to Take Action, Simon Sinek maintains that we are loyal to companies and products or inspired by individuals because of how they make us feel. We often cannot describe these feelings adequately, but the source of this loyalty is related to a consistent vision or message that evokes in us an emotional response within the limbic system of the brain. Consistent with this view, our members clearly respond to the ACCP vision with enthusiasm, contributing time and energy to ACCP because they view this organization as their professional home. ACCP is committed to providing a high level of service to members who share our vision for clinical pharmacists being truly accountable for optimal medication therapy in the prevention and treatment of disease. In this regard, ACCP serves as the only organization driving the development, advancement, and positioning of clinical pharmacists. Our members have shown their commitment to the organization―908 members volunteered for ACCP committee service this year. I was able to place 253 members on this year’s committees. Although many of you were undoubtedly disappointed by not being selected to serve, you have my gratitude, and I hope you will apply again. In addition to the work discussed earlier, this year’s committees will be addressing the impact of potential changes in the Medicare benefit on those who practice in the acute care environment, developing an acute care survival guide, and considering new technology and methods for CMM provision to patients at remote locations. Other committees will be describing methods for evaluating the outcomes of resident teaching certificate training, designing a certificate program for the research training of residents, and describing measures to better support residency preceptors and program directors. These are ambitious tasks for the year, and I look forward to their completion.
We will continue to set and strive to achieve high standards of practice for ourselves and for our organization, patients, students, and researchers. Thank you for giving me the opportunity to serve ACCP as we kick off another year dedicated to advancing clinical pharmacy.
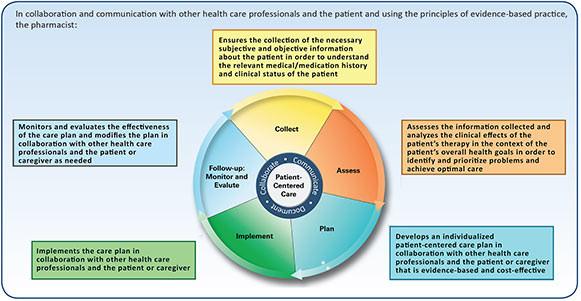
Figure. The 2014 JCPP Pharmacist Process of Care.