I would like to begin by thanking the College for the great privilege of serving as your president for the coming year. It is the pinnacle of my professional career. As with most things in life, one does not get here without a lot of mentoring, a lot of support, some chiding, and a lot of love from family, friends, and colleagues. I have worked with many exceptional clinical pharmacists over the years and have been able to advance my skills through these relationships. Of course, for me, as I suspect for many of you as well, some of my greatest teachers have been my patients. Their perseverance and unwavering spirit at the most difficult times of their lives is inspiring and humbling.
And that brings me to my theme for this year: Medication Optimization Across the Care Continuum.
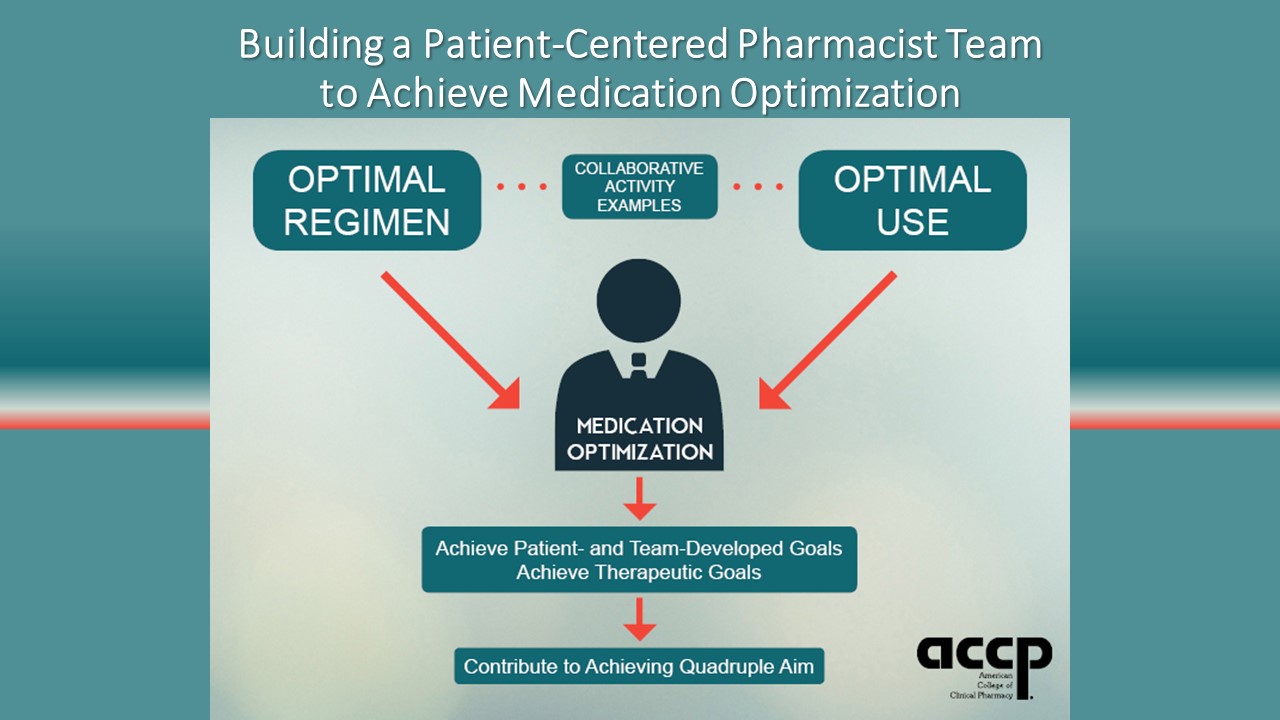
The goal of my theme is to communicate the essential need for the standard of practice for clinical pharmacy to be consistent across ALL practice settings. The theme was inspired by a presentation at the 2017 ACCP Annual Meeting Town Hall in Phoenix that resonated with me, “Engaging Community Pharmacists. Three Cs: Communicate, Coordinate, Collaborate.” The presenters described community pharmacists and practice-based clinical pharmacists partnering through communication, coordination, and collaboration to provide direct patient care through the development of “enhanced services networks.” In this presentation, patient-centered pharmacist teams worked together across the care continuum to optimize medication regimens and use to achieve patients’ therapeutic goals through medication optimization.
ACCP should be at the forefront of ensuring medication optimization, fostering the provision of a standard practice for patient care by a clinical pharmacist regardless of the practice setting – ambulatory, acute care, or community. Moreover, the process and level of care should always be the same in each setting. Our patients deserve it and should demand it. I would argue that ACCP is the best organization to advance and promote this standard of practice. The College sought to advance clinical pharmacy at its inception 40 years ago, and this is still its mission. However, whereas clinical pharmacy was mainly practiced in the inpatient setting at that time, it is now practiced in a variety of settings, including the community. We only have to look at the College’s current vision for the profession of pharmacy:
- Most pharmacists will provide direct patient care and participate in other clinical activities.
- The standard of practice in any health care setting will hold pharmacists responsible for medication optimization.
As part of its strategic plan, ACCP is exploring mechanisms to establish pharmacist collaborations across different care settings that achieve medication optimization. Eventually, the College hopes to form a strategic alliance that promotes effective and scalable collaborative pharmacy practices across the care continuum.
The Institute for Healthcare Improvement (IHI) recently released a report titled No Place Like Home: Advancing the Safety of Care in the Home (www.ihi.org/resources/Pages/Publications/No-Place-Like-Home-Advancing-Safety-of-Care-in-the-Home.aspx). This IHI initiative partners pharmacists with providers to improve patient safety. The report states that “community pharmacists possess an untapped potential for ensuring medication safety in the home, but their involvement is limited in most communities.” In this regard, the report also notes that medication safety represents a significant concern in the home setting, especially among patients with complex medication regimens for chronic illness. Pharmacists in the community should have the expertise to detect drug-related problems and adverse events. Moreover, pharmacists should optimize medications across the care continuum. Along these lines, the IHI report outlines the collaborative work of Community Care of North Carolina (CCNC) and the Community Pharmacy Enhanced Services Network (CPESN), noting that CCNC patients see their community pharmacist an average of 35 times per year, whereas they see their primary care provider only 3 times per year.
ACCP is engaged with CPESN and the National Community Pharmacists Association Innovation Center in this type of initiative, key features of which include:
- Collaboration of pharmacists from medical practices and community-based pharmacies to leverage resources and information to optimize patients’ medications and improve the quality of their care.
- Achievement of medication optimization by optimizing medication regimens (via CMM) and optimizing medication use (via enhanced services).
- Pharmacists’ participation in the drafting of a consensus guidance statement for successful collaboration across settings.
Several sessions at the Global Conference have been devoted to medication optimization and CMM.
In recent years, emphasis has been placed on transitions of care and how patients are vulnerable during these transitions. Often in such transitions, medications are not reconciled, patient education is not optimized to ensure adherence, and procuring medications may be challenging. If we think about our own practices for a moment, we should be asking how we’re currently ensuring when our patients are discharged from an inpatient admission or clinic visit, how their medications are optimized, and how they will attain therapeutic goals. Moreover, how do we ensure their medications will continue to be optimized when they are back home and in the community? I suspect that for many of us, the answer is unclear. Yet, as noted earlier, our patients deserve a consistent standard of practice from pharmacists that optimizes their medications and achieves the best possible outcomes, no matter where they encounter us.
Many of our 2019 committees will address issues related to medication optimization across the care continuum, including using best practices in care transitions and implementing CMM through telehealth practices. I would like to thank all the members who volunteered this year to serve on committees and task forces. The real work and advancement of the College occurs through their efforts. I look forward to continuing this dialogue with you over the coming year. Let’s all work to see what we can achieve together toward the goal of Medication Optimization Across the Care Continuum. Thank you for the great honor of serving as the College’s president as we embark on our 40th anniversary.